Introduction: Sickle cell anemia (SCA) is highly prevalent in sub-Saharan Africa with >300,000 annual births, and substantial morbidity and mortality due to limited resources. The burden of stroke in this population is of particular concern, given the devastating clinical and neurocognitive sequelae of these events. Hydroxyurea, a potent disease modifying therapy for SCA, is safe and feasible for low-resource and malarial endemic countries within sub-Saharan Africa and when used at maximum tolerated dose (MTD), decreases the incidence of acute painful vaso-occlusive events, infections, malaria, transfusions, hospitalizations, and death. Whether hydroxyurea can prevent primary stroke in SCA within Africa has not yet been determined, due in part to lack of stroke screening programs using transcranial Doppler (TCD) ultrasonography. If effective, hydroxyurea would have even more therapeutic benefits for children with SCA, particularly in settings where blood is not available, affordable, or safe. We designed the Stroke Prevention with Hydroxyurea Enabled through Research and Education (SPHERE) trial to determine the stroke risk among Tanzanian children using TCD screening and to investigate the effects of hydroxyurea to reduce that risk.
Methods: The SPHERE trial (NCT03948867) is a single center prospective phase 2 open-label screening and treatment pilot study at Bugando Medical Centre, a teaching and referral hospital in Mwanza, Tanzania. Children 2-16 years old with SCA consented to TCD screening by locally trained and certified examiners; recent febrile illness, red cell transfusion, or hospitalization were temporary exclusions. Study participants with maximum Time-Averaged Mean Velocity (TAMV) on TCD exam categorized as conditional (170-199 cm/sec) or abnormal (≥200 cm/sec) are offered hydroxyurea with escalation to MTD, while those with normal TCD screening exams will be rescreened annually. Hydroxyurea is initiated at ~20 mg/kg/day using 500 mg capsules and a weekly dosing calculator, then escalated every 8 weeks by 5 mg/kg/day up to 35 mg/kg/day. Children on hydroxyurea are seen monthly during dose escalation and every 3 months after reaching MTD. The primary endpoint is change in TCD velocity after 12 months of hydroxyurea therapy. Secondary endpoints include changes in splenic volume and filtrative function; change in renal function; incidence of infection, especially malaria; hydroxyurea pharmacokinetics; and genetic modifiers of disease including pharmacogenomics.
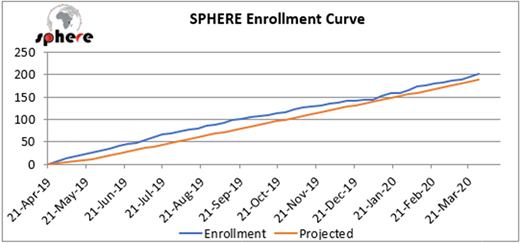
Results: From April 2019 to April 2020, a total of 202 children underwent TCD screening, exceeding the projected enrollment pace and goal (Figure). The average age (mean ± SD) at enrollment was 6.8 ± 3.5 years, and 53% were female. A majority had previous dactylitis (75%), painful vaso-occlusive episode (93%), blood transfusion (68%), and malaria (89%). Recurrent hospitalization was common with 30% having >5 previous hospitalizations. Only 4% had previously used hydroxyurea. Baseline labs included hemoglobin = 7.8 ± 1.3 g/dL, HbF = 9.3 ± 5.4 %, and ANC = 5.5 ± 2.4 x 109/L. Baseline assessment revealed a palpable spleen in 46 children (23%), and most of these (29) were ≥5 cm below the costal margin. Abdominal ultrasonography documented splenic tissue in 91% of children with an average volume of 101 ± 123 mL (range 8-1045). TCD examinations were performed in all children at enrollment with average TAMV of 148 ± 27 cm/sec [median 144, IQR 130-169 cm/sec] with 76% normal, 21% conditional, 2% abnormal, and 1% inadequate exams. Of 47 children eligible for hydroxyurea for elevated TCD velocities, 45 successfully initiated treatment, while 1 lived too far away for regular visits, and 1 had low blood counts from acute splenic sequestration and died before initiating study treatment.
Conclusion: Children with SCA in Tanzania have a high risk for primary stroke. Identification of elevated TCD velocities through screening by local trained certified examiners, coupled with initiation of hydroxyurea treatment with dose escalation to MTD, offers a feasible and affordable means by which to lower TCD velocities and reduce primary stroke risk. Now fully enrolled, SPHERE has built local clinical capacity, research infrastructure and high-quality TCD screening, and will prospectively determine the benefits of hydroxyurea for stroke prevention, as a prelude for expanding hydroxyurea access for children with SCA in Tanzania.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal